Functional Apps
Part of the Orthodontics Poster Collection
A functional appliance in orthodontics refers to a device used primarily in the treatment of growing patients to utilize the forces of the masticatory muscles (the muscles used in chewing) to produce desired orthodontic effects and changes in the jaws. These appliances are typically used to correct bite discrepancies, such as Class II malocclusions, where the upper jaw and teeth are positioned ahead of the lower jaw and teeth.
1. Rationale
The rationale for using functional appliances in orthodontics lies in their ability to harness the natural growth potential and the neuromuscular forces of a growing patient to correct discrepancies between the upper and lower jaws. Particularly in cases of Class II malocclusions, where there's a relative protrusion of the upper jaw or retrusion of the lower jaw, functional appliances can either stimulate favourable growth in the mandible (lower jaw) or restrict unwanted growth in the maxilla (upper jaw), bringing the jaws into a more harmonious relationship. Their use during the patient's growth spurt can capitalize on the biological adaptability of the skeletal structures, potentially reducing the need for more invasive treatments, like orthognathic surgery, later in life. Moreover, by improving the skeletal relationship early, they often pave the way for simpler orthodontic tooth alignment procedures in the subsequent phases of treatment.
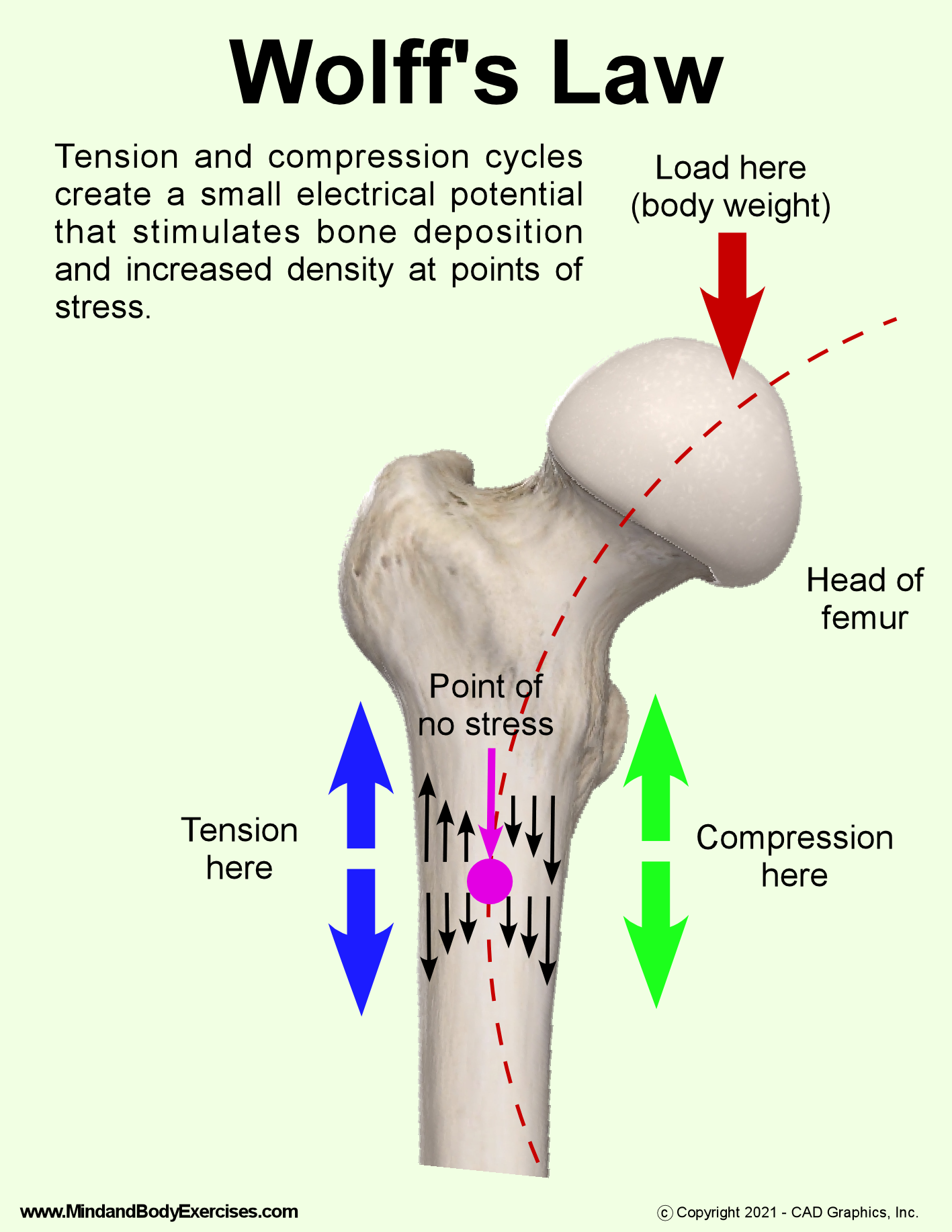
Wolff's Law is a principle of orthopaedics that was introduced in the 19th century by the German anatomist and surgeon, Julius Wolff. The law states that bone in a healthy person or animal will adapt to the loads under which it is placed. If a bone is subjected to increased loading, it will remodel itself over time to become stronger and better suited to resist that type of loading. Conversely, if a bone is not subjected to regular loading or stress (such as in cases of limb immobilization), it will become weaker due to the decrease in bone density.
In essence, Wolff's Law underscores the dynamic nature of bone tissue, emphasizing that it's continuously being broken down and rebuilt in response to the mechanical forces applied to it. This principle is foundational in orthopaedics and biomechanics and has implications for areas like fracture healing, bone adaptation in athletes, and the prevention of bone loss in situations like prolonged bed rest or space travel and also orthodontics.
The Functional Matrix Theory is a concept in craniofacial biology that provides an understanding of the growth and development of the facial skeleton. Proposed by Melvin Moss, this theory posits that the growth of the skeletal structures (like bones) is secondary and responsive to the growth of the surrounding functional soft tissues and spaces.
The theory is built upon two primary components:
Functional Matrix: This refers to the soft tissues and functional components, including the brain, eyes, tongue, airways, and muscles, which require space and dictate the size and shape of the craniofacial structures.
Skeletal Matrix: This is the supporting component, consisting of the bones and cartilages. According to the theory, these skeletal structures grow and adapt in response to the needs of the functional matrix.
For example, the growth of the brain would necessitate an increase in the size of the cranial vault, or the growth and functional needs of the tongue and developing dentition would influence the shape and size of the mandible and maxilla.
In essence, the Functional Matrix Theory emphasizes that the growth and development of the craniofacial skeleton are largely influenced by the functional needs and demands of the soft tissues and spaces they encompass and support.
2. Method of Action
Functional appliances in orthodontics work by harnessing and redirecting the natural forces generated by the muscles of mastication and the surrounding soft tissues to facilitate desired changes in the dentoalveolar and skeletal structures. Their method of action can be understood in the following ways:
Postural Change: Many functional appliances work by holding or guiding the mandible (lower jaw) into a more forward position. This postural shift induces a stretch in the surrounding muscles, especially the muscles of mastication.
Muscular Adaptation: With the change in jaw position, the muscles adapt to this new posture. This adaptation creates a changed pattern of muscular forces acting on the teeth and the jaws.
Stimulation of Growth: By holding the mandible forward, there's a potential to stimulate increased growth at the condyle (the growth centre of the mandible located at the back near the joint). This can lead to a lengthening of the mandible in cases of mandibular deficiency.
Restriction of Growth: In cases where the maxilla (upper jaw) is growing too far forward, the functional appliance can exert backward-directed forces on it, potentially slowing down or redirecting its growth.
Dental Changes: Apart from skeletal effects, functional appliances can induce dentoalveolar changes. For instance, protrusive upper incisors can be up righted, or retroclined lower incisors can be proclined, helping to correct the bite.
Altered Functional Matrix: As per the Functional Matrix Theory, changes in the surrounding soft tissues can influence skeletal growth. Functional appliances can modify the functional environment (like tongue posture, muscle function, or airway space) and indirectly affect skeletal development.
Remodelling of Temporomandibular Joint (TMJ): With the forward positioning of the mandible, there can be adaptive changes or remodelling in the TMJ, facilitating the maintenance of the new jaw position.
The effectiveness of functional appliances depends on various factors including patient age, growth potential, appliance design, and patient compliance. Typically, they are most effective during the patient's growth spurt when the potential for skeletal adaptation is highest.
Mode of Action of Functional Appliances
-forward posture of the mandible
-condyle held forward in the fossa
-condylar effects
-remodelling of the glenoid fossa
-soft tissue elasticity
-effects on dentition
-effects on skeletal structures
-altered neuromuscular activity
-differential tooth movement
-dentoalveolar tipping
-lower incisor proclination
-upper incisor distal tipping
-lower molar mesial tipping
-upper molar distal tipping
-expansion
-vertical opening
-guidance of eruption to some degree
3. Classification
Functional appliances in orthodontics can be classified based on various criteria, such as their design, mode of action, or whether they're fixed or removable. Here's a broad classification:
Based on Retention:
Removable Functional Appliances: These can be taken out of the mouth and are typically worn for a specified number of hours per day. Examples include:
Twin Block
Bionator
Activator
Frankel appliance (Functional Regulator)
Fixed Functional Appliances: These are attached to the teeth and cannot be removed by the patient. Examples include:
Herbst appliance
Jasper Jumper
Forsus Fatigue Resistant Device
MARA (Mandibular Anterior Repositioning Appliance)
Based on Mode of Action:
Tooth-borne Appliances: These primarily engage the teeth to exert their effects. Example: Bite Jumping Appliance or BJA.
Tissue-borne Appliances: These primarily engage the surrounding tissues like the mucosa and have minimal engagement with teeth. Example: Frankel appliance.
Combined tooth-tissue borne Appliances: These engage both teeth and surrounding tissues. Example: Twin Block.
Based on the Direction of Force Application:
Anteroposterior Correctors: These correct discrepancies in the front-to-back relationship of the jaws, e.g., Twin Block, Herbst appliance.
Vertical Correctors: These modify vertical growth patterns, e.g., Bite-blocks.
Transverse Correctors: These address width discrepancies of the dental arches or jaws, e.g., Schwarz appliance for arch expansion.
Based on the Functional Mechanism:
Muscle Training Appliances: These are designed to retrain and harness the muscles for orthodontic purposes. Example: Myofunctional appliances.
Growth Modifying Appliances: These aim at modifying the growth potential of the jaws, e.g., Twin Block or Herbst appliance.
4. Indications
Class II Malocclusion: Functional appliances are commonly indicated in cases with Class II malocclusion, especially when it's due to a retrusive mandible.
Growing Patients: These appliances are most effective during the growth spurt, where the potential for skeletal adaptation is high.
Mandibular Retrognathism: When the lower jaw (mandible) is set back relative to the upper jaw (maxilla).
Favourable Growth Pattern: They're best indicated for patients with an average to horizontal growth pattern. Vertical growers (with long face syndrome) may not benefit as much and might even experience increased vertical growth, which might not be desirable.
Mild to Moderate Skeletal Discrepancies: Functional appliances are especially useful for patients with mild to moderate skeletal discrepancies. Severe discrepancies might need surgical intervention.
To Reduce Need for Extraction: In some cases, functional appliances can reduce or eliminate the need for tooth extractions in orthodontic treatment.
To Reduce Need for Surgery: Early intervention with functional appliances can, in some cases, minimize or eliminate the need for orthognathic surgery later on.
5. Contraindications
Non-Growing Patients: Functional appliances rely heavily on growth potential. They're generally contraindicated for patients who have completed their growth.
Class III Malocclusions: These appliances aren't typically indicated for Class III malocclusions (where the mandible is ahead of the maxilla). However, there are other types of appliances designed specifically for Class III corrections.
Severe Skeletal Discrepancies: In cases of severe skeletal discrepancies, functional appliances might not offer the desired correction, and surgical intervention might be more appropriate.
Unfavourable Growth Patterns: Patients with a strong vertical growth pattern may not be ideal candidates for certain functional appliances, as they might exacerbate the vertical growth.
Patients with Temporomandibular Joint Disorders: Some functional appliances can alter the position of the mandible and might exacerbate TMJ symptoms.
Poor Patient Compliance: The success of many functional appliances, especially the removable ones, is heavily dependent on patient compliance. If a patient is unlikely to wear the appliance as instructed, it might not be the right choice.
Dental Health Issues: Patients with significant untreated dental health problems, like severe periodontal disease or rampant caries, may not be suitable candidates until these issues are addressed.
6. How to take a bite registration
A precise bite registration is vital for the effectiveness of any functional appliance. The construction bite details how the device should sit within the patient's mouth. This data is essential for shaping the appliance, and guiding the forces to induce the desired dental and skeletal modifications. The following aspects must be captured in the bite:
Midlines: Align the skeletal midlines correctly. Use the maxillary and mandibular labial frenum as reference points.
Vertical Opening: The degree of bite opening depends on the patient's overbite. Regardless of specific measurements, ensure there's a gap of at least 5 to 6 mm between the premolars, ensuring proper engagement of the upper and lower components. Optimal outcomes often arise from even wider openings, ensuring the patient interacts with the blocks instead of bypassing them.
Forward Movement of the Lower Jaw (Protrusion): For most Class II situations, begin where the lower front teeth are slightly ahead of an edge-to-edge position. The protrusion should be ample, allowing for some overcorrection since the final results tend to fall short of the appliance's design. Adjust based on the patient's overjet, growth tendencies, and age. Those with vertical growth patterns or mature patients generally need less forward movement compared to those with horizontal growth patterns or those in the mixed dentition phase. Adjust the bite registration accordingly.
Materials:
• Polysiloxane putty (condensation silicone) - a better option than wax
• PVS bite registration material (as an alternative choice)
• Wooden popsicle stick - more suitable than a plastic bite fork but the ExactoBite can be used
Steps:
With the teeth slightly separated to negate any occlusal disturbances, use a red wax disposable marker to draw lines on the top and bottom front teeth. This provides a clear reference to ensure the bite captures the midlines correctly.
Position a wooden popsicle stick vertically between the top and bottom midlines to determine the vertical and forward measurements. Carve small V-shaped notches into the popsicle stick to mark the position of each arch and their midlines. Typically, in cases where the lower jaw is slightly ahead of an edge-to-edge position, the V-notch for the bottom jaw will be somewhat ahead of the top jaw's notch.
Guide the patient in practicing how to open their mouth widely and shift their lower jaw directly forward into the designated V-notch or bite fork, making sure the midlines are aligned consistently. The movement of the lower jaw should be direct and forward without any side shifts.
Prepare the polysiloxane putty, using a generous amount of catalyst to expedite the setting. Shape the putty into a cylinder and then mould it into a U shape. Place this over the lower teeth. Carefully position the popsicle stick over the U-shaped putty and guide the patient to shift their lower jaw, aligning the V-notch with the top teeth. As an alternative, you can introduce the PVS bite material into the bite space using a dispensing tool.
Ask the patient to stay motionless while the bite material solidifies. In the interim, push any extra putty towards the patient's teeth to ensure a snug fit.
Once set, inspect the bite to confirm the correct midline alignment, vertical spacing, and forward positioning.
7. How to choose an appliance
In practice this is usually decided by clinicians based on where they trained as well as who trained them. However, this should not be the fundamental method.
Choosing a functional appliance in orthodontics involves a comprehensive assessment of the patient's needs and specific characteristics. The decision process is influenced by clinical findings, desired outcomes, patient's compliance, age, and growth status, among other factors. Here's a general guideline to help you make an informed decision:
1. Assessment of Skeletal and Dental Discrepancies:
Identify the type of skeletal discrepancy: Class II (typically a retrusive mandible) or Class III (protrusive mandible or retrusive maxilla). Evaluate the severity of the discrepancy: Mild, moderate, or severe.
2 . Age and Growth Status:
Functional appliances work best during periods of active growth. Utilize growth prediction methods, like hand-wrist radiographs or assessment of secondary sexual characteristics, to determine the growth status. Adult patients or those nearing the end of growth are less responsive to functional appliances.
3. Type of Malocclusion:
Determine the nature of occlusal discrepancies, like deep bite, open bite, crossbite, etc. Consider the amount of overjet, overbite, and molar relationship.
4. Patient Compliance:
Removable appliances require high patient compliance. If patient cooperation is questionable, a fixed functional appliance might be more appropriate.
5. Desired Direction of Force:
Some appliances can be more vertically or horizontally directed in their force application, so understanding the growth pattern (vertical vs. horizontal) is crucial.
6. Specific Features of the Appliance:
Some appliances, like the Twin Block, allow freedom of movement and are more comfortable, whereas others, like the Herbst, are fixed and provide constant force. Consider the appliance's adjustability and ease of management.
7. Treatment Goals:
If dentoalveolar changes (movements of teeth within the bone) are primarily desired, certain appliances might be more appropriate. If significant orthopaedic (jaw) changes are the primary goal, other appliance choices might be more suitable.
8. Consideration of Side Effects:
Some appliances might cause unwarranted side effects, like excessive vertical facial growth or unwanted dental movements. Choose an appliance that minimizes these side effects for the specific patient.
9. Ease of Fabrication and Management:
Some appliances are simpler to fabricate and adjust. Depending on the orthodontist's familiarity and the laboratory's capabilities, certain appliances might be preferred
10. Previous Successful Outcomes:
Often, orthodontists tend to favour appliances they've had success with in the past.
11. Patient Comfort and Aesthetics:
Consider appliances that are more comfortable for the patient and have less visual impact, especially if aesthetics is a concern.
Lastly, always engage in open communication with the patient (and parents, if the patient is a minor) to ensure they understand the treatment options, potential benefits, limitations, and any possible side effects. The final choice should ideally be a collaboration between the orthodontist's expertise and the patient's preferences and needs.
8. Twin Block
The Twin Block is a popular removable functional appliance in orthodontics, specifically designed to treat Class II malocclusions, often characterized by a retrusive mandible (lower jaw). Developed by Dr. William Clark in Scotland during the early 1980s, this appliance consists of two separate plates: one for the upper jaw and one for the lower jaw. These plates have inclined planes, or "blocks", that interlock when the patient bites down, encouraging the lower jaw to move forward into a more advanced position. The design of the Twin Block ensures that every time the patient bites or swallows, they facilitate the desired forward positioning of the mandible. Over time, this promotes favourable orthopaedic and dentoalveolar changes, helping to correct the jaw relationship and align the teeth. One of the major advantages of the Twin Block is its patient-friendly design, offering better comfort and allowing more natural jaw movements than some other functional appliances.
9. Monoblock
The Monoblock appliance, often used in orthodontics, is a one-piece functional device designed primarily to address Class II malocclusions associated with a retrusive mandible (backward positioned lower jaw). Unlike the Twin Block, which consists of two separate plates for the upper and lower jaws, the Monoblock is a single unit that encompasses both arches. This design encourages the mandible to adopt and maintain a forwardly positioned posture, thereby aiding in the correction of the skeletal discrepancy. The appliance aids in achieving both dentoalveolar and skeletal modifications, promoting the forward growth of the mandible and potentially adjusting the position of the teeth within their respective arches. However, due to its one-piece design, the Monoblock may be perceived as bulkier and less comfortable for some patients, especially when speaking or eating. Despite this, its efficacy in harnessing the growth potential, especially in younger patients, makes it a valuable tool in orthodontic treatment planning.
10. Andreson Activator
The Andresen Activator is a functional orthodontic appliance named after its developer, Karl Hawley Andresen, who introduced it in the 1930s. This removable appliance is primarily designed to treat Class II malocclusions associated with a retrusive mandible. Unlike many traditional orthodontic devices that focus on moving teeth, the Andresen Activator aims to modify jaw growth and function by repositioning the lower jaw forward. It is constructed from acrylic and covers both the upper and lower dental arches, with a large space in between for the tongue, promoting a more forward tongue posture. When the patient closes their mouth, the lower jaw is encouraged to advance, adjusting its relationship to the upper jaw. The appliance also has protrusive springs and a labial bow to guide tooth movement. Patients are advised to wear the Andresen Activator during the evening and night, and its passive design capitalizes on the involuntary swallowing mechanism to generate the desired orthopaedic effect. Over time, the consistent forward positioning of the mandible can lead to favourable skeletal and dentoalveolar changes.
11. Harvold Activator
The Harvold appliance, also known as the "activator," was developed by Erling Harvold in the mid-20th century and is one of the classic removable functional appliances in orthodontics. Primarily designed to treat Class II malocclusions associated with a retrusive mandible, the Harvold appliance works by holding the lower jaw in a forward position to encourage adaptive growth and development. The appliance, made of acrylic, encompasses both the upper and lower dental arches. Its design is passive, without any screws or active components, relying on the natural functions of the jaw—such as swallowing—to provide the necessary stimulus for change. By positioning the mandible forward and maintaining this posture over time, the appliance capitalizes on the body's adaptability, leading to both skeletal and dentoalveolar changes that help correct the Class II discrepancy. The Harvold appliance laid the groundwork for various other functional appliances and remains a testament to the principles of functional therapy in orthodontics.
12. Medium Opening Activator
The Medium Opening Activator is a specific type of functional orthodontic appliance that aims to address Class II malocclusions, often stemming from a retrusive mandible. As its name suggests, this activator is characterized by a medium opening between the upper and lower dental arches, which serves dual purposes: it encourages the forward positioning of the mandible while also allowing room for the tongue, promoting a more favourable tongue posture. Constructed primarily from acrylic, the Medium Opening Activator covers both dental arches and functions passively, relying on natural jaw movements, especially swallowing, to exert its therapeutic effects. By holding the mandible in a forward position, this appliance facilitates adaptive skeletal and dentoalveolar changes over time. Moreover, by providing space for the tongue, it aids in addressing dysfunctional swallowing patterns and tongue thrusts, ensuring a more holistic approach to orthodontic treatment. The appliance is typically worn during the evening and night-time hours, capitalizing on involuntary jaw functions for maximum therapeutic impact. This is helpful in mixed dentition treatments.
13. Bionator
The Bionator is a functional orthodontic appliance designed primarily to correct Class II malocclusions resulting from a retrusive mandible. Originating from the principles of Balters' philosophy in the mid-20th century, the Bionator facilitates the forward positioning of the lower jaw, promoting harmonious jaw growth and development. Constructed from acrylic, the device encompasses both the upper and lower dental arches, with ample space provided for the tongue to ensure a natural and improved posture. Unlike some other functional appliances, the Bionator is relatively less bulky, which can enhance patient comfort and compliance. When worn, the appliance utilizes the forces generated during swallowing and other jaw movements to encourage the mandible to grow in a more forward direction, thereby addressing the skeletal discrepancy of a Class II relationship. Additionally, by guiding the jaw and influencing the tongue's posture, the Bionator can affect both skeletal and dentoalveolar changes, making it a versatile tool in the orthodontist's armamentarium.
14. Dynamax
This functional appliance was used previously and is another functional appliance used to correct Class II bites. However due to multiple issues with emergencies this appliance has been relatively not used any more.
15. Frankel
The Frankel appliance, often referred to as the functional regulator, is a unique orthodontic device developed by Dr. Rolf Frankel in Germany during the 1960s. Unlike traditional orthodontic appliances that directly move teeth, the Frankel appliance primarily focuses on altering the function and behaviour of the surrounding oral and facial musculature to effect skeletal and dental changes. Its design comprises a series of acrylic pads, shields, and labial bows that aim to free the teeth from the potentially detrimental influences of the perioral muscles, thereby allowing them to erupt and align in a more favourable environment. By doing so, the appliance seeks to harness the natural forces of the facial muscles to guide the jaws and teeth into more harmonious positions. Particularly beneficial for growing patients with Class II or Class III malocclusions, the Frankel appliance is known for its emphasis on promoting proper tongue posture, lip competency, and nasal breathing, thereby addressing both the functional and aesthetic aspects of orthodontic treatment.
16. Herbst
The Herbst appliance is a well-established fixed functional orthodontic device designed primarily to treat Class II malocclusions, which are often characterized by a retrusive mandible or lower jaw. Introduced in the early 20th century by Dr. Emil Herbst and later refined over the decades, this appliance utilizes telescopic attachments connecting the upper and lower jaws to facilitate the forward positioning of the mandible. Unlike removable functional appliances, the Herbst appliance is cemented or banded to the molars and remains active continuously, ensuring consistent mandibular advancement day and night. The constant anterior positioning of the lower jaw encourages adaptive changes both in the temporomandibular joint and in the dental arches. Over time, this results in favourable skeletal and dentoalveolar modifications, bringing the jaws and teeth into better alignment. Due to its fixed nature, the Herbst appliance offers the advantage of bypassing the compliance issues often associated with removable devices, making it a preferred choice in many clinical scenarios.
17. Jasper Jumper
The Jasper Jumper is a fixed functional orthodontic appliance designed to address Class II malocclusions, typically arising from a retrusive mandible. Introduced by Dr. Joseph Jasper in the 1980s, this appliance operates on the principle of connecting the upper and lower dental arches via a small, telescopic spring-loaded mechanism. The Jasper Jumper exerts a continuous force to propel the mandible forward, aiming to correct the jaw discrepancy and improve the Class II relationship. Unlike some other functional appliances that require patient compliance, the Jasper Jumper is directly attached to the braces, offering a more consistent treatment force and often leading to quicker results. The device is appreciated for its compact design, reducing the potential for tissue irritation and enhancing patient comfort. Over time, by maintaining the lower jaw in a more forward position, the Jasper Jumper promotes favourable dentoalveolar and potentially skeletal changes, facilitating the correction of the malocclusion.
18. Forsus
The Forsus Fatigue Resistant Device is a contemporary fixed functional appliance used in orthodontics to correct Class II malocclusions, often associated with a retrusive mandible. Introduced as an alternative to traditional headgear and elastics, the Forsus device provides a consistent, continuous force to advance the mandible, thereby improving the relationship between the upper and lower jaws. Consisting of a spring coil module that attaches to the upper molar bands and the lower arch wire, the Forsus device is designed to be both efficient and comfortable for patients. Since its integrated with fixed braces, the need for patient compliance, often a concern with removable appliances, is mitigated. Its continuous force application not only accelerates treatment time but also minimizes the adverse effects like root resorption. The Forsus device represents the evolution of orthodontic appliances, offering an effective, patient-friendly solution to a common orthodontic challenge.
19. Twin Block Points
· These are the important aspects of the Twin Block
· The twin block consists of 2 parts (the lower and the upper)
· When the appliance is placed in the mouth and the patient tries to close, the only way possible is to wear it in class III incisal relation (protrude the jaw), this moves the teeth (proclines lowers and distalizes uppers)
· Please note that a labial bow is not always needed.
On the fit appointment:
· Measure the overjet at centric relation and record
· Fit the upper first
· Ensure the clasps clip into the undercuts of the teeth and there is good retention
· Make sure the patient understands how to remove it, always from the posterior clasps never from the front or it will break
· Once both appliances are in tell the patient to occlude
· The bite blocks should hit on each other
· The upper and lowers should occlude on the bite block only
· Now tell the patient to posture the lower jaw forwards so that the appliance will fit ahead of the upper as in diagram
· There should be an anterior open bite when both the appliances are in the mouth of approximately 3-4 mm.
· They must both be worn for any effect to occur approximately 16-20 hrs per day
· They should not be worn during eating or sports
· This means the patient has to wear the appliance to sleep. It is challenging at first but soon patient will adapt.
· The patient and guardian must be behind the treatment, or it will fail.
· The main dropout rate of this appliance is due to poor cooperation and poor enthusiasm from both the patient and the guardian.
· Usually, speech and saliva will be affected in the beginning, and these are usually adapted within 4 weeks.
· Ensure the appliance is cleaned twice a day.
· The patient should be able to remove and fit it by themselves.
· Patient should always be in a protrusive position to allow the appliance to work.
· They should try their best to attain lip competence as well.
Review appointments
· Review the patient every 4 weeks in the first instance to ensure compliance
· The average reduction of the overjet is 1-2mm per 6 weeks and would be quicker at younger ages.
· Lateral open bites are important indicator of wear
· The bite blocks can be trimmed towards the end to allow some
· Expansion can be activated as crossbites manifest
· Overjets and overbites should be measured at each review
Transition procedure
Difficult to predict anchorage demands, allows some occlusal settling, there may or not be postural adaptation of the condyle, expansion loss is possible, some relapse may occur at this stage. Fixed appliances can be placed with or without anchorage reinforcement.
Options
· 1) Straight away fixed appliances
· 2) Night-time wear of the functional
· 3) No wear of the functional
· 4) Headgear only